Regulations
As technology advances across all healthcare fields, Software plays a significant role in all products. It is widely integrated into digital platforms serving both medical and non-medical purposes. Medical device software is one of three types of Software related to medical devices. The other two types of medical device software include Software that is an integral part of the medical device (medical device software) and Software used in manufacturing or maintaining the medical device. Software...
Cybersecurity for Medical Devices – FDA and EU MDR Perspective
FDA –Food and Drug Administration The revolution in the digital sector has resulted in the Internet of Things (IoT), Software as a Medical Device (SaMD), Internet of Medical Things (IoMT) and other connected devices permeating the healthcare environment, both in hospital and home, has ended up with the possibility of cyberattacks and intrusions against the connected medical devices and the networks to which such a device is connected. Most Medical devices are connected to the Internet, hospita...
Article 61 Clinical Evaluation in the EU MDR
Article 61 Clinical Evaluation The MDR reinforces the clinical data and evaluation process (article 61 and Annex XIV), and the manufacturer must confirm the device’s conformity to fundamental health and safety requirements using reliable clinical data and evaluation. The clinical evaluation establishes the device’s safety and capacity to fulfil its intended function. It also evaluates adverse side effects and determines whether the benefit-risk ratio is acceptable. Manufacturers must...
Regulation (EU) 2017/746 (IVDR): MDR IVDR Amendment Jan. 2023
Introduction Recent amendments to Regulation (EU) 2017/745, also known as the Medical Devices Regulation (MDR), have introduced significant changes to the timelines and conditions for placing certain medical devices on the market or putting them into service. This comprehensive analysis explores the key points of these amendments, focusing on the intricate timeline considerations. Paragraph 3 Amendments Paragraph 3 has undergone crucial revisions, introducing new provisions (3a to 3g) that...
EU MDR Unveiled: What You Need to Know About Medical Device Regulation in Europe
Introduction about Medical Device Regulation in Europe Introducing the Medical Device Regulation in Europe addresses several challenges. It aims to enhance medical device regulation in Europe to ensure a higher level of safety and effectiveness. The need for the MDR arises from various factors, including shortcomings identified in the previous regulatory framework (Medical Device Directives) and the evolving landscape of medical technologies. Rapid technological advancements in the field of medi...
Importance of Human Translations vs Machine Translations
Human translation Human translations produce accurate results because it involves at least one language expert. Translations, with a human touch to them, are precise because of the in-depth knowledge that translators carry Human translations are done by native speakers of a particular language or people certified in language translations . Therefore, it is culturally diverse, nuanced and is of high quality. However, this high-quality product is expensive. Machine translation Machine transla...
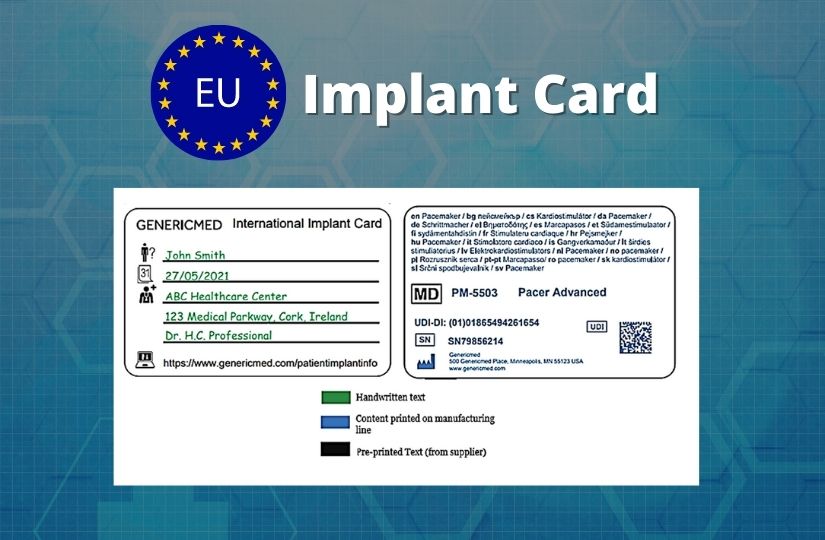
Implant Cards for Europe
The European Union’s Medical Device Regulation (MDR 2017/745) introduces a new requirement for manufacturers producing implant cards for medical devices. As per EU MDR, implantable devices are any devices, other than the active implantable devices, that are partially or completely implanted into the human body or are used to replace an epithelial surface or the surface of the eye, by clinical intervention, and are meant to stay in place after the procedure. The device that is intended to be pa...
Top 7 Guidance On Class I Medical Devices
The EU MDR 2017/745 imposes more stringent requirements for Class I devices. Under the new regulations, Manufacturers must righty classify a medical device and provide technical documentation following the device class. The risk class under MDD could change under MDR. In some cases, medical devices could be up classified from Class I medical devices to Class II a/b medical devices or Class III medical devices. Please read our article on the classification of medical devices to understa...
Updates in ANVISA GMP 2022 document
Agência Nacional de Vigilância Sanitária – ANVISA is the Regulatory Body of Brazilian government. What is Good Manufacturing Practice (GMP)? Good manufacturing practices are the procedures that must be followed in order to comply with the guidelines set forth by regulatory agencies that oversee the authorization and licencing of the manufacture and sale of medical devices. The GMP document released on 30th March 2022 for Medical and IVD produ...
Nomenclature of Medical Devices
Medical device nomenclatures are those products used to prevent, diagnose, treat, and monitor the many diseases known to humankind. Medical devices and medicines play an equally important role in treating human beings. To learn more about medical devices, read our article on the definition of a medical device. This article discusses the nomenclature of medical devices and examples of these. What is the Nomenclature of Medical Devices? To simply put it, the nomenclature is the naming of a me...